Exemptia - World’s First Adalimumab Biosimilar
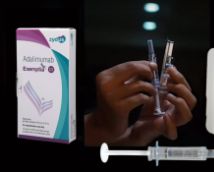
Adalimumab, trade name Exemptia, is a potent TNF-inhibitor and anti-inflammatory drug manufactured and promoted by Zydus Group in India. Adalimumab works as anti-TNF, blocking over production of TNF and its harmful effects on the body. It’s prescribed to people who have Rheumatoid Arthritis, Ankylosing Spondylitis, Psoriatic Arthritis and to children having Juvenile Idiopathic Arthritis from a Rheumatologist. The usual dosage for Rheumatoid Arthritis is 40mg once in every 2 weeks.